Light seen by the eye is sent through the optic nerve, a cable of nerve fibers connecting the eye with the brain. The tip of the optic nerve that enters the eye, called the optic nerve head or optic disc, can be seen by looking into the eye with a special device called an ophthalmoscope, Figure 1.
Figure 1. Normal optic nerve head and retina
Optic disc drusen are small collections of protein-like material in the optic nerve head, that can be found in 1 to 2 of every 100 people. In most cases they are found in both eyes. Optic disc drusen are probably congenital, meaning that they are already there at birth, but it is currently unknown exactly why they form. In childhood, drusen are usually buried deep down in the optic nerve head. As the drusen get bigger and the optic nerve fibres thin with age, the drusen become more obvious and eventually visible with an ophthalmoscope. Optic disc drusen usually become visible during the teenage years.
How can optic disc drusen affect vision?
Optic disc drusen usually do not affect vision and people live completely normal lives without ever realizing they have drusen. However, peripheral vision loss may occur slowly, go unnoticed by the patient and only become detected at a so-called automated visual field examination at a regular eye examination.
Less commonly there may be a sudden, painless blurring or loss of a part of the visual field. This could be due to a compression of or decreased flow through a blood vessel in the optic nerve head caused by optic disc drusen, a so-called drusen-associated ischemic optic neuropathy. A rarer complication from optic disc drusen is a so-called choroidal neovascular membrane, which is a collection of abnormal blood vessels growing under the retina near the optic nerve. If these abnormal vessels bleed, they can cause a sudden visual loss.
How are visible optic disc drusen diagnosed?
When drusen can be seen with the ophthalmoscope, they are easily diagnosed, Figure 2. The examination typically reveals optic disc elevation, blurred optic disc margins without obscuration of retinal blood vessels, and a lumpy-bumpy appearance of the optic disc border.
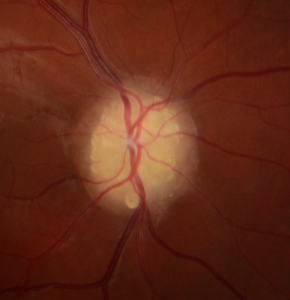
Figure 2. Visible optic disc drusen
How are buried optic disc drusen diagnosed?
When optic disc drusen are buried within the optic nerve head, as is often the case in children, they may be difficult to detect and distinguish from a true swelling of the optic disc, Figure 3. A true swollen optic disc can be a sign of a serious and potentially life-threatening increase of the pressure in the brain. In that case the swollen disc is called papilledema.
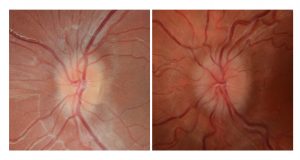
Figure 3. Buried optic disc drusen (left) and optic disc swelling caused by raised intracranial pressure (right)
To distinguish between buried drusen and a mild degree of papilledema, it is sometimes not enough for the doctor to use an ophthalmoscope. If the drusen contain calcium, and are large enough, they can usually be picked up by various imaging methods such as ocular ultrasound, autofluorescence or CT scans. Optical coherence tomography (OCT) is an imaging method increasingly used to detect optic disc drusen, Figure 4, even the ones that are small, deeply buried and uncalcified.
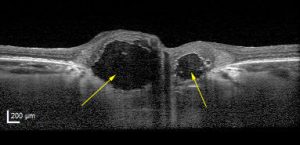
Figure 4. OCT scan of the optic nerve head showing 2 large optic disc drusen (arrows)
How are optic disc drusen treated?
There is currently no effective treatment for optic disc drusen. However, treatment of drusen-associated complications may be indicated and determined by the clinical context in which the patient presents. Severe drusen-associated visual field defects may cause driver license restrictions depending on national laws and regulations.
